
RECOGNISING THE EARLY SYMPTOMS AND CAUSES ALLOWS YOU TO PROTECT YOUR JOINTS

Joint pain
This is pain in one or more of the body’s joints, such as the knee, shoulder, elbow, wrist, hand, hip, ankle and foot.
It can easily occur when the joint capsule or the ligaments are subject to excessive traction. In this case, the structure of the joint cartilage can alter, therefore limiting its ability to withstand loads and shear stress. For example, a pain in the knee after a strain or after sports could be caused by a traumatic injury to the meniscal fibrocartilage or by kneecap instability.
Joint pain, along with factors such as family history, unhealthy lifestyle and older age, could be a symptom of arthritis, a chronic degenerative and disabling disease that has a major impact on the patient’s quality of life, functioning and social life, as well as on healthcare systems
Osteoarthritis (OA)
The disorder is characterised by regressive focal alterations of the hyaline cartilage of the synovial joints, preceded by decreased water content, degradation of extracellular matrix, altered formation of glycosaminoglycan chains, and decreased chondroitin sulfate compared to keratan sulfate. A quantitative reduction in the synthesis of hyaluronic acid and in its molecular weight results in changes in the rheological properties of the synovial fluid.
These phenomena generate chondral lesions, and the loss of joint cartilage increases the friction between the ends of the two joint bones, thus altering/deforming the subchondral bone.
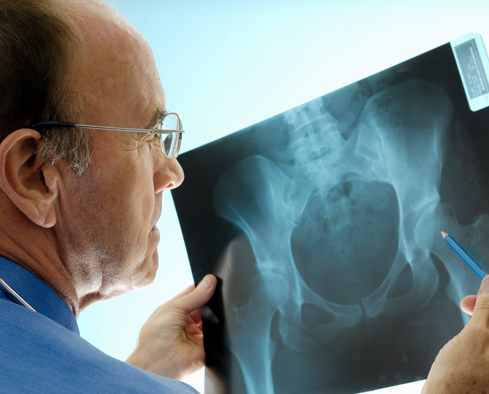
Ranking at the top of the list of painful syndromes with a high social cost, today the disorder is considered by many as a heterogeneous group of morbid conditions with common histopathological and radiographic features.
Due to recent developments in terms of prevention and therapy, this condition is no longer regarded as an inevitable consequence of aging, but rather as a disease that can be prevented and managed by working on lifestyle, risk factors, early diagnosis and the adoption of an appropriate therapy.
Risk factors for osteoarthritis
It is well known that the risk of developing arthritis increases with age, although significant differences have been observed between arthritis and cartilage aging. Causes can be linked either to genetic factors (non-modifiable) or to lifestyle habits (modifiable).

OLDER AGE
Senescence is associated with a progressive loss of elasticity and resistance to stress, thereby potentially favouring damage to the cartilage tissue.

SEX
Women are more likely to develop osteoarthritis, especially in the knee and the small joints of the hands.
FAMILY HISTORY
Increasing importance is given to genetic factors and a family history of arthritis, especially along the female line of descent.
MECHANICAL FACTORS
Excessive joint load can occur, for example, as a result of bone deformities, occupational and sports activities, traumatic injuries or microtrauma.

OBESITY
Being overweight and obesity are significant modifiable risk factors for arthritis, due to excessive joint load and mechanical factors.
Possible symptoms
From a clinical standpoint, osteoarthritis is polymorphic and may be associated with several signs and symptoms.
Pain is the main symptom reported by patients suffering from osteoarthritis, and is generally also the main reason why patients seek medical advice. The pain starts off as a dull ache, and only manifests itself after prolonged activity.
However, as the disease progresses, joints may hurt at rest and at night. This pain relates to the inflammation of the synovial membrane, and may or may not be associated with muscle contraction.
Joint stiffness in the morning, after a night rest, or after a period of inactivity is short-lived: it normally lasts 10-15 minutes, and almost never exceeds half an hour.
Functional limitation is progressive, but sometimes only manifests at advanced stages of the disease. It is not merely a result of joint space narrowing, but also of reflex muscle contractions.
A hard swelling is the most significant tell-tale sign of arthritis. Nodules are almost always limited to the hands and are not usually painful. In other joints, they are very rare and not necessarily linked to osteophytes. Soft swelling may occur in the event of joint effusion. Tenderness to palpation is generally associated with structures surrounding the joint.
Crepitus, or a popping noise, is a common sign of arthritis upon palpation, during active and passive motion. It is due to irregular and often minimally lubricated joint surfaces that lie close to each other due to joint space narrowing, thereby causing joint wear and tear.
Understanding different types of joint pain and osteoarthritis
There can be two types of joint pain: mechanical stimuli, originating from mechanical changes in the environment of the joint (eg, through direct trauma), and chemical stimuli caused by inflammation.
Whatever the cause, there may be an impaired use of the muscles and tendons, resulting in a specific disorder.
Joint pain, along with other factors, could be a symptom of osteoarthritis. The Italian Society of Rheumatology (SIR, 1999) has classified two forms of the disease:
primary and secondary osteoarthritis, depending on whether or not there is an identifiable underlying cause.
The areas most affected are: lumbar spine (33%), cervical spine (30%), knee (27%), and hip (25%).
Joint pain
WHERE IT IS FOUND
It is found in the dermis (the thickest skin layer), in joint cartilage, in the synovial fluid that fills the joint cavities, in tendons, and in the vitreous body of the eye.
WHAT IT DOES
It improves the hydration, consistency and elasticity of tissues, and is a key player in wound healing and in normal joint function. Moreover, it also helps manage many feminine inconveniences or discomfort.

Understanding different types of joint pain and osteoarthritis
WHERE IT IS FOUND
It is found in the dermis (the thickest skin layer), in joint cartilage, in the synovial fluid that fills the joint cavities, in tendons, and in the vitreous body of the eye.
WHAT IT DOES
It improves the hydration, consistency and elasticity of tissues, and is a key player in wound healing and in normal joint function. Moreover, it also helps manage many feminine inconveniences or discomfort.
Preventing pain and the onset of the disease
Although considerable progress has been made in understanding the pathogenetic mechanisms of osteoarthritis (OA), as yet there is no definitive cure for this disease.
Osteoarthritis is the result of the combination of several risk factors that can cause cartilage damage. Assessing the risk factors – in particular genetic factors, which have been shown to increase the likelihood of developing the disease – is a key element of prevention.
As time passes, we are increasingly exposed to risk factors, and this leads to the onset of joint disorders.
Prevention of osteoarthritis and joint pain takes place on 2 levels.
Primary prevention aims at preventing the disease from developing. To this end, it is important to:
- Keep your body weight in check: being overweight and obesity are well-recognized risk factors, especially to the knee. A healthy diet helps maintain your ideal body weight and promotes proper nutrient absorption.
- Improve posture and reduce excessive, repetitive overloads. Repetitive trauma suffered during youth may be responsible for the onset of osteoarthritis at an advanced age.
- Engage in proper physical activity, it reinforces the muscles that support the joints, without overexerting them.
- Avoid all activities with a high impact on the joints or any sports that involve repetitive movements. Repetitive mechanical stress leads to alterations in the cartilage structure and metabolism.
Secondary prevention aims at preventing the disease from progressing. To this end, nutraceuticals and food supplements containing glucosamine and chondroitin sulfate may be helpful. Being constituents of the cartilage matrix, they may prove effective in preventing or delaying the onset of joint disorders.
The latter should not be underestimated, if we think, for example, that advice to rest the affected joint is helpful to manage pain: in the case of load-bearing joints, such as the hip and knee, it relieves the joints of pressure and harmful mechanical factors.
Moreover, proper exercise is also important, both for the treatment of joints and to avoid subsequent trauma.